Metabolic Evaluation
Patients of all ages with inborn errors of metabolism (IEMs) are diagnosed and treated through the Metabolic Specialty Care Center (SCC) at Miller Children’s.
Approved CCS Center
The Metabolic Center at Miller Children’s is a California Children’s Services (CCS) approved Special Care Center (SCC). This means a specially designated multidisciplinary care team is responsible for all care coordination and case management of a patient in this program. Patients typically qualify for the Metabolic CCS Special Care Center by medical diagnosis, complexity of their disease and financial status.
Diagnosis
IEMs affect the way in which either proteins, fats or carbohydrates are utilized in the body for energy, growth or function of normal metabolism. Diagnosis of IEMs is now primarily through newborn screening following the expansion in 2005 of the number of amino acid disorders and organic acid disorders identified through the California newborn screening program. However some IEMs still remain to be clinically diagnosed. Life-long dietary management is the principal means of management for IEMs.
Miller Children’s Metabolic Center receives patients, who have tested positive during the newborn screening process. The Metabolic Center also treats adults who are a part of the Genetically Handicapped Persons Program (GHPP).
Clinical Evaluation
Once the baby or the child comes to the Metabolic Center the geneticist and metabolic care team performs a diagnostic evaluation and psychodevelopmental assessment to determine how to create a care plan to manage the metabolic disorder for patients and their families. Prenatal counseling is also available.
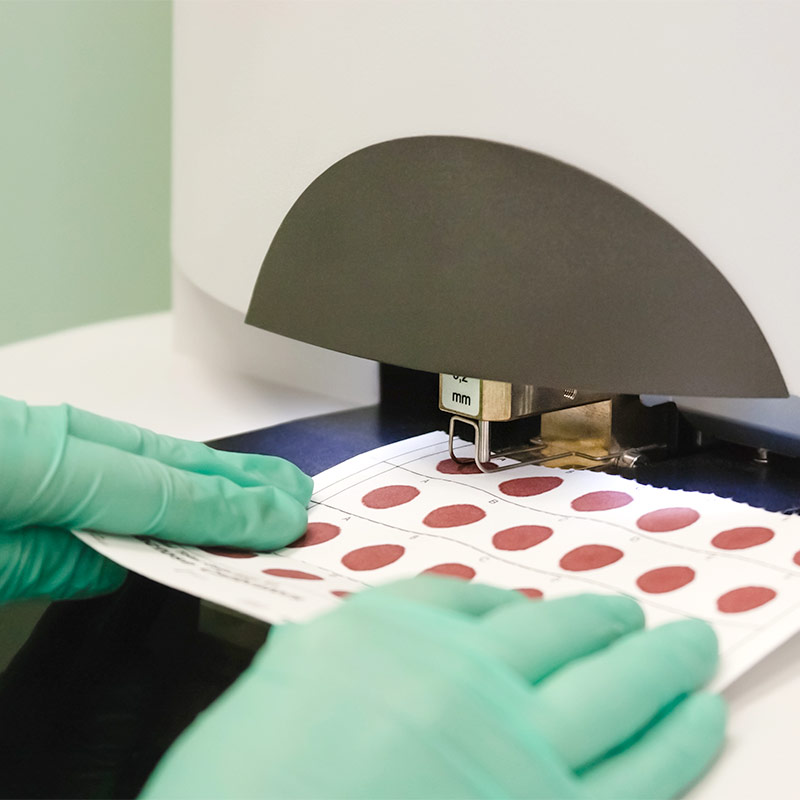
Symptoms of IEMs are quite varied but usually are associated with a more prolonged recovery than expected following a common viral illness. Diagnosis of an IEM not identified through newborn screening is done through a review of a patient’s history, physical examination and specialized blood and urine tests. DNA analysis is then often utilized to confirm a clinically suspected IEM.
Amino Acid Disorders (AAD)
Amino acid disorders are hereditary disorders caused by poor amino acid processing in the body. This results from the body’s inability to metabolize or breakdown certain amino acids in proteins, or by the inability to detoxify the by-product of amino acids through the urea cycle. These disorders cause symptoms early in life, so newborns are routinely screened for several disorders, such as phenylketonuria (PKU), maple syrup urine disease, homocystinuria and tyrosinemia. The lack of early identification and treatment may result in serious medical consequences, including mental retardation, developmental delays, and/or death.
Organic Acid Disorders (OAD)
Organic acid disorders are a group of rare inherited conditions. Enzymes are needed to process protein from food, problems with one or more of these enzymes can cause an organic acid disorder. Children with organic acid disorders cannot break down protein properly causing harmful substances to build up in their blood and urine. These substances can affect health, growth and learning. Most of these disorders have severe forms that present in the first week of life and usually result in a neonatal emergency. Infants are usually well at birth, but develop poor feeding habits, irritability, lethargy, vomiting, metabolic acidosis, ketosis or coma.
Fatty Acid Oxidation Disorders (FAOD)
Fatty acid oxidation disorders are a group of rare inherited conditions. A number of enzymes are needed to break down fats in the body, problems with any of these enzymes can cause a fatty acid oxidation disorder. People with FAODs cannot properly break down fat from either the food they eat or from fat stored in their bodies, which can result in excessive fat buildup in the liver, heart and kidneys. This buildup can cause a variety of symptoms, ranging from hepatic failure, encephalopathy, heart and eye complications to general problems with muscle development.
Metabolic Therapy
Treatment & Condition Management
Therapy for IEMs is principally through dietary management. An amino acid, a specific fat, or a specific carbohydrate is usually limited, but not eliminated, through the evaluation and guidance of the metabolic dietitian. The metabolic dietitian’s expertise and experience leads to a dietary prescription supporting normal growth and development while limiting the specific food component of the diet that leads to an accumulation of an illness-causing compound. Usually a small amount of the specific food component is necessary for normal growth and function, but a normal amount causes illness. For many IEMs a specific dietary formula is prescribed to assist in supporting normal growth and development. Management is through periodic clinic appointments with the Metabolic SCC team (metabolic dietitian, nurse, social worker, and physician) and telemedicine between a member of the team and the patient or family.
The metabolic dietitian at the Metabolic SCC at Miller Children’s will coordinate with the family’s local health care providers to assist the patient in following dietary guidelines and prescriptions. The metabolic dietitian assists the child’s school district to prepare appropriate foods for the school lunch as required under federal law for each child with a disability. Periodic cooking classes with an emphasis on preparing low-protein foods are offered to enable the family and patients to more effectively manage their disorder.
Conditions
Type 1 diabetes, or insulin-dependent diabetes, is an incurable auto-immune disease. Type 2 diabetes, or non-insulin dependent diabetes, is the most common form o
Your Care Team
Other Team Members
- Metabolic Dietitian
- Nurse
- Social Worker
- Physician