How COVID-19 Can Affect Your Child’s Heart
Announcer
This is weekly dose of Wellness brought to you by MemorialCare health system. Here's Deborah Howell hello and welcome to the show.
Deborah Howell
I'm Deborah Howell and today we're going to find out how COVID-19 affects a child heart. Our guest today is Doctor Saar Danon Medical Director, Pediatric cardiology and congenital cardiac catheterization at MemorialCare, Miller Children’s and Women’s Hospital Long Beach. Welcome Doctor Dannon.
Saar Danon, M.D.
Thank you and thank you for having me on your podcast.
Deborah Howell
Lovely to have you today. How can a COVID-19 diagnosis cause multisystem inflammatory syndrome or MIS-C?
Saar Danon, M.D.
Yeah, so interestingly, MIS-C is something that we're still learning, learning a lot about. It's a relatively new diagnosis as is obviously COVID-19 in general and it causes inflammation in multiple organ systems and in someone that's previously had some kind of exposure to COVID-19 so the mechanism of that is still being really worked out, but it seems to be related to the body's immune response to having previously been exposed to the virus. So, it's really an immune reaction that causes the symptoms of MIS- C.
Deborah Howell
Got it and can you explain this MIS-C a little bit more.
Saar Danon, M.D.
Like I mentioned, it's a new diagnosis as we know the global pandemic with COVID-19 began in late 2019 and into 2020. Interestingly, in the United Kingdom in April, they started noticing previously healthy children that had severe inflammation in multiple organ systems. It was similar to something that we previously had known. A Disease called Kawasaki Disease, and these clinicians really deserve a lot of credit because they saw something they really have never seen before. Similar to another disease process, but definitely with unique characteristics and were able to discern that these patients had previous exposure or suspected exposure to COVID-19, and this was back in April in 2020 and then in May of 2020 we started to see similar cases in New York and the whole community. The medical community got together and were able to really define this syndrome and figure out that this is a new entity that we need to learn about. Some children are severely affected, and as I mentioned, we're still learning about it. There's multiple publications every month regarding MIS-C
Deborah Howell
Very interesting, and as you said, very good work by those clinicians. So do we know what causes MIS-C and what are the symptom?
Saar Danon, M.D.
Right, so the cause of MIS-C is some kind of immune response. There's a specific definition that the CDC has laid out for what MIS-C really is, and the definition is really any person under 21 years of age that presents with signs of inflammation like fever, laboratory evidence of inflammation and is severely ill requiring hospitalization with involvement of two or more organ systems, and that can involve the heart, the kidneys, the lungs, the blood, the gastrointestinal system, the skin and the brain and the other part of the definition is 2 things. One, there's no other explanation for this and two, that the patient has a prior diagnosis or current diagnosis of the COVID-19 or a suspected previous exposure within the last four weeks. So that's how we are defining MIS-C and as far as the symptoms in the clinical presentation, it definitely varies from patient to patient. Patients will develop a fever and that's one of the hallmarks characteristics but as we know, a lot of things in Pediatrics that cause fever. The other part is having a involvement of the GI tract and that can involve abdominal pain, vomiting, or diarrhea. It also will involve the skin so you can develop a rash or other skin findings and not just the outer skin. Even the inner skin, like the mucocutaneous regions like the inside of the mouth or the eyes and things like and then in its most severe form, they can present in shock meaning low blood pressure. What we call low cardiac output state where they're not getting sufficient blood to their organs, and those patients are obviously severely ill.
Deborah Howell
And how do you go ahead and diagnose MIS-C?
Saar Danon, M.D.
So it is a clinical diagnosis. Unfortunately there's no one test that can say if someone has MIS- C, so it has become a difficult diagnosis. It is similar to other things like I mentioned particularly Kawasaki disease. For MIS- C. The way we diagnose it is really if someone has a clinical picture like those symptoms that we described and also has the lab markers or inflammation, we have different lab tests that we can do to show that there is inflammation going on in the body, and then the other part that's really important again, in the absence of another infection or disease that would explain everything and then the prior exposure. So if we can get a definitive test to show that someone either is currently test positive for COVID-19 with one of the vial test or previously tested positive that is very helpful in the diagnosis, but sometimes we can test to see if there's antibodies present from a prior exposure or we will just use a history where the patient was in contact with someone that had COVID-19 or was suspected of having COVID-19 so it is a clinical diagnosis.
Deborah Howell
And what do parents do if they suspect their child has MIS- C?
Saar Danon, M.D.
If parents suspect that their child has MIS-C, the first thing obviously is to contact their pediatrician. They can start the work up, but if these patients are particularly sick, if their symptoms are severe. If they're really concerned, the best thing is to bring them to the closest urgent care or emergency department where they can have a full evaluation.
Deborah Howell
And how does MIS- C affect children of different ages, doctor?
Saar Danon, M.D.
To the diagnosis of MIS-C. Because of what the term means, the multisystem inflammatory syndrome in children we use that really to define the diagnosis in kids. So, anyone under the age of 21 years, but it can affect them all ages or I should say similar presentation in all ages. But what we see is in all the diagnosis of MIS- C is that the patients are most likely to be between age of 6 to 12 years, so those are the most likely ages. That doesn't mean that we don't see it in under six years in over 12 years of age, but those are the ones that are most commonly affect.
Deborah Howell
And then after 21 it goes from being MIS- C for children to MIS-A for adults.
Saar Danon, M.D.
So that's good. I haven't seen that in the publications, but I will submit that as a possible adult diagnosis.
Deborah Howell
I was just throwing that out there.
Saar Danon, M.D.
I'll give. You credit for it, yeah?
Deborah Howell
OK, thank you. I appreciate that I'm in a medical journal. All right. Why is it important for a child who had MIS-C See to see a pediatric cardiologist?
Saar Danon, M.D.
Because MIS-C can affect the heart and cause inflammation of the heart, it's very important to figure that out as early on in the course as possible. So, like the inflammation that happens in other organ systems, the most severe organ system that is affected is the heart, and there's two main things that we see. One is it can affect the heart function where the ventricles that actually squeeze and pump blood outside of the heart are not functioning normally, so the blood can't get to where it needs to get throughout the body, so decrease in what we call the cardiac function. Action is something that can obviously be very significant, very severe, and what can cause those symptoms that are shocked that I mentioned. The other thing that we can see is enlargement or dilation of the coronary arteries, the arteries that supply blood to the heart. Those are called coronary artery aneurysms and that may not develop any symptoms, but those kids risk for developing clots in their coronary arteries and actually developing what we call minor cardio infarction or a heart attack by losing blood flow to their heart. So, it's really important to have that evaluation as part of the evaluation for MIS- C or suspected MIS- C and that way the cardiologists could evaluate the function of the heart, the coronary arteries, and both of those can be evaluated by something called an echocardiogram, and ultrasound of the heart. The other thing is to make sure that none of this causes rhythm, abnormalities, and sometimes that can be diagnosed with an electrocardiogram or EKG. Although MIS-C has a very specific diagnosis and what I mentioned to make the diagnosis of the patient has to be severely ill and hospitalized, we do see patients that maybe don't meet the exact clinical criteria for MIS-C but do have some degree of what we call clinical or subclinical inflammation in the heart. And sometimes they may have very nonspecific symptoms Things like chest pain or palpitation, meaning faster, irregular heartbeats so we do see kids that maybe had a prior exposure. Don't meet the exact definition, but they do have these nonspecific symptoms, so it is important that they're evaluated as well and have the same EKG and echocardiogram and possible lab testing to look for that so in general that can be done by a pediatric cardiologist.
Deborah Howell
OK, now the big and final question. How is MIS-C treated and what's the prognosis of children affected by it?
Saar Danon, M.D.
Yes, so because MIS-C is such a variable presentation, it's very patient specific and it depends on the individual child and how they present the most severe form is when they do develop shock or heart failure, meaning the heart is not getting the blood that the body needs in order to carry out the normal function. In those cases, the kids may be severely ill and needs heart medications and even continuous drips of medications. Sometimes it affects the rest or system the lungs, and they may need to be intubated, meaning on a mechanical ventilator and really support those organ systems. If the kidneys are affected, and obviously that's something that needs to be addressed and then really what we would consider supportive treatment. Really just making sure they remain hydrated are being monitored closely and get the appropriate treatment that they need. We do use sometimes steroids, and something called intravenous immunoglobulin to treat these kids. So, it really is dependent on how sick they are and what organ systems are involved? As far as the prognosis that you asked, the good news is that these patients usually do very well. Even the most severe cases usually will have a full recovery. There's actually a paper that just got published about a week ago, and it showed that even in the most severe cases where we see the heart is affected with the corner. Aneurysms and the cardiac dysfunction about 91% of those patients had full recovery in less than 30 days, so most patients do recover, so overall, the good news is if patients get the appropriate treatment, the prognosis is very good.
Deborah Howell
Well, that is fantastic news indeed. Thank you so much Doctor Danon for being on our show today and for shedding some light on this syndrome. It's been really great talking to you.
Saar Danon, M.D.
Thank you again for having me. It's been fun.
Deborah Howell
Our pleasure to learn more about the Children Heart Institute. Go to millerchildren.org/heart or call 855-999-6241 to make an appointment. And if you enjoyed this podcast and would like to hear more, just go to memorialcare.org/podcasts. I'm Deborah Howell. Thanks for listening and have yourself a fantastic day.
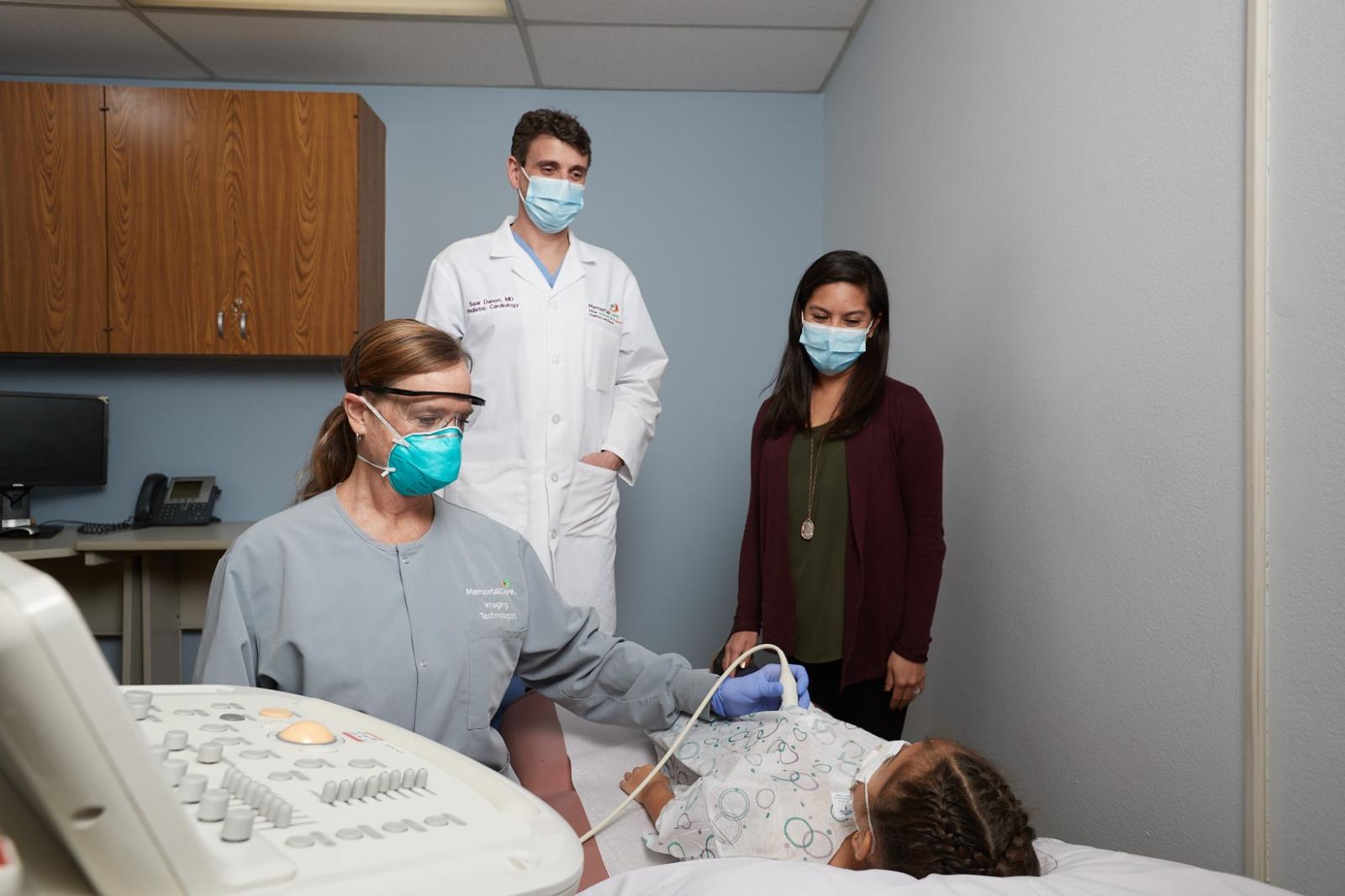
Researchers have learned that children who have been infected with COVID-19 can later experience cardiac effects due to Multisystem Inflammatory Syndrome (MIS-C). This can occur weeks after exposure to COVID-19, and in some cases without symptoms during the initial infection. MIS-C is a condition where multiple organ systems become inflamed, including the heart which can cause damage to the heart cells.
Listen to the podcast featuring Dr. Saar Danon above.
Featured Speaker:
Dr. Saar Danon, medical director, Pediatric Cardiology and Congenital Cardiac Catheterization, Children's Heart Institute, Miller Children’s & Women’s Hospital Long Beach
Related Providers