We're one of 22 hospitals in California to feature a regional Level IV NICU, which is the highest designation available by the American Academy of Pediatrics. This means we have advanced capabilities, along with skilled specialists, to care for sick and critically ill, and premature babies. We treat nearly 1,200 critically ill and premature babies each year.
The NICU is home to the largest Small Baby Unit in the region to care for extremely low birthweight babies in an environment mimicking the womb, including an Tiny Baby Program.
The NICU is just down the hall from our Cherese Mari Laulhere BirthCare Center. If a woman has a high-risk pregnancy, where the baby may need to go to the NICU immediately following birth, they will not need to be taken away from mom and transported to another hospital.
Miller Children’s & Women's has a full range of advanced neonatal medical care, including state-of-the-art diagnostic and surgical care, complete with leading technologies and care techniques, including whole-body cooling for brain development and bubble c-pap to increase oxygen flow.
Programs
Miller Children’s & Women’s and the March of Dimes have collaborated to provide a program to support families during their hospital stay. Since it can be very difficult to spend many days or weeks in the hospital. The Program offers families support through activities, education and parent-to-parent mentoring.
NICU Parent Mentor Program Offers:
- Bedside activities
- Mentoring from another parent who has shared a similar experience
- Creative activities in the NICU Family Center, especially during the holidays
- Information and comfort for families with premature and critically ill newborns being cared for in the NICU at Miller Children’s & Women's
- Professional photography
NICU Family Center
In the NICU Family Center, there is an education area for parents to learn more about their child’s condition, a sibling area designed to provide entertainment and distraction, private lockers and family work stations. The room serves as a hub for the March of Dimes NICU Parent Mentors so families can have direct access to someone that has gone through a similar experience. The mentors also host
Parent Hour – where parents can decorate their babies’ first onesie or create their very first picture frame – giving them time to clear their mind.
The NICU has lactation consultants and lactation educators who also are registered nurses with many years of NICU experience. These dedicated consultants have helped many new moms successfully breastfeed their NICU babies.
Benefits of NICU Lactation Consultants
Lactation consultants provide individualized consultation and assistance. Through consultation, the team helps moms provide expressed breast milk and/or breastfeed their baby/babies during hospitalization and longer. The goal is to support efforts to provide breast milk and make the transition to breastfeeding before the family goes home.
Human Milk Lab
Our Human Milk Lab, part of our Clinical Nutrition Department, is a centralized area where breast milk and formulas are prepared. Our Human Milk Lab collects, stores, prepares and delivers expressed breast milk and pasteurized human donor milk to our NICU patients.
If a mother desires to provide breast milk to her premature infant, but is unable to, then pasteurized human donor milk may be provided for eligible NICU patients. Pasteurized human donor milk is milk that has been donated by mothers who have extra breast milk. This is milk is thoroughly tested and undergoes a pasteurization process before it can be frozen and utilized in various facilities.
The health benefits of using pasteurized human donor milk include:
- Infection fighting factors
- Active growth and development hormones
- Ideal nutrition
- Easier digestion
At Miller Children’s & Women’s joins the American Academy of Pediatrics and the World Health Organization in recommending breast milk as the best feeding option for babies. By having an on-site Human Milk Lab, we are able to immediately provide breast milk to a baby in the NICU if deemed appropriate by the neonatologist.
Mothers who donate extra milk go through a rigorous screening process. Once approved, their donated human milk is heat treated (pasteurized), destroying all bacteria, viruses and white blood cells. Many enzymes, growth factors, immune factors, vitamins and minerals are unchanged or only slightly decreased. Babies are individually assessed for eligibility.
Contact Us:
Lactation consultants can be reached at (562) 661-1901 for appointment scheduling and phone consultations.
The NICU at Miller Children’s & Women's has an Integrated Transitional Care Area for newborns that need the most attention and require extended care. The Integrated Transitional Care Area within the NICU ensures that patients with a severe diagnosis or pending procedures and surgeries receive special attention and care.
The care team assigned to each patient stays with him or her throughout their stay, which establishes a much-needed consistency of care for families during treatment. Not limited to just NICU nurses and physicians, the Integrated Transitional Care Area care teams utilize a variety of professional caregivers who work together with a patient’s family to plan for each baby’s unique case. These care teams often include occupational therapists, physical therapists, dietitians, palliative care specialists, case managers, social workers, family educators, pharmacists and any other specialized care team members that may be needed.
- Certified Hearing Screening Center
- Child Life Program/Sibling Support
- Comprehensive Surgical Care
- Donor Milk Program (exclusive human milk)
- Infant CPR Training for Parents/Family
- Neonatal Cardiac Program
- Neonatal/Perinatal Research Program
- Neonatal Continued Care Program
- Outpatient Specialty Care Centers, Clinics & Programs
- Palliative Care
- Parent Education & Support Program (Bilingual-Spanish)
- UCI Physician Residency Training/Neonatal
- Whole Body Cooling Program
The Women, Infant and Children (WIC) Program at Miller Children's & Women's Hospital Long Beach is a supplemental food and nutrition program for income eligible pregnant, breastfeeding, and postpartum women and children under age five. Participants in the WIC Program are provided with food vouchers that can be used to purchase specific nutritious foods, which are high in protein and/or iron. The WIC Program is a service of the City of Long Beach Department of Health and Human Services, Nutrition Services Division.
WIC Program Services
- Nutrition Education.
- Medical Care Referrals.
- Breastfeeding Support/Education.
- Classes in car seat safety, baby bottle tooth decay, prenatal care and infant safety.
- Services available in English, Spanish and Cambodian.
WIC Program Participants
- Women who are pregnant, breastfeeding or have recently given birth.
- Infants or children under the age of five years (depending on funding).
- Women who breastfeed are eligible to stay on WIC for 12 months after baby’s birth.
- Women who do not breastfeed are eligible to stay on the program for six months after baby’s birth.
- Pregnant women must provide verification of pregnancy.
- Participants must also provide current medical information for all applicants.
Supportive Care
Miller Children’s & Women's offers a variety of support programs to help families while their infant is in the NICU.
Every parent wants to be with their baby at all times, especially in the overwhelming environment of the NICU. However, babies may be in the NICU for as long as three months and with other children, jobs that they can’t leave for an extended time, etc. they can’t be there full time. Working and busy parents take great solace in the fact that if they can’t be at the hospital during daytime hours, NICU “cuddlers,” who are hospital trained, are there to provide that “human touch” so desperately needed by all babies, especially those in the NICU.
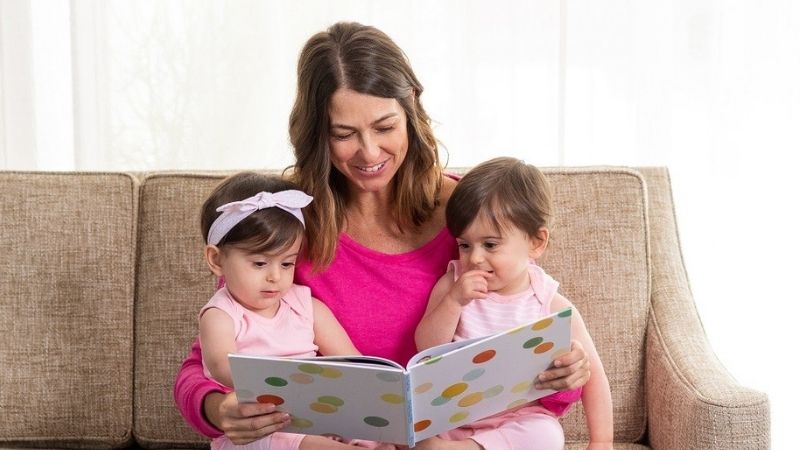
The “cuddlers” provide therapeutic talk and touch – they don’t feed, change diapers or walk around with the babies. They simply hold them, read to them or quietly singing to them. It is required that the NICU “cuddlers” hold them for a minimum of 45 minutes up to four consecutive hours, providing the infant comfort and appropriate stimulation. The work the “cuddlers” do helps preemies grow faster, so they can go home to their families sooner.
NICU “cuddlers” have to go through extensive classroom and bedside training, beyond what is required of a typical volunteer. “Cuddlers” maintain strict hand washing, infection control and practices while in the NICU, and adhere to all hospital policies and confidentiality.

The Cherese Mari Laulhere Child Life Program at Miller Children’s & Women's works to make a NICU stay more comforting for NICU babies and their families.
One of Child Life’s key components when supporting NICU babies and their families is supporting the sibling(s) of the NICU patient. A Child Life Specialist can sit down with a sibling and talk to them about what kind of medical equipment they may see on their little brother or sister and answer any questions the sibling may have before they visit. This helps normalize the hospital environment and alleviate possible anxieties.
Siblings of NICU patients also are given a scrapbook to document their visits to the hospital. The scrapbook helps them understand the NICU environment and helps familiarize language they may hear in the hospital. Parents are encouraged to go through the scrapbook with the sibling to help with the coping process.
Child Life Specialists encourage parents to interact with their baby by reading books and singing to them to aid in bonding – especially when they aren’t able to hold the baby. The Child Life Program includes music therapists, who create a variety of sounds using instruments and singing to stimulate the brain and help with the patient’s developmental growth.
The music therapists at Miller Children’s & Women's work with families one-on-one to teach the benefits of music therapy. Families also can write songs for their baby with a music therapist and record them on a CD to take home as a memory.
Once a NICU patient is finally ready to go home, the Child Life team provides a certificate for nurses to fill out with the patient’s, weight and length at discharge compared to when they were born to see how the baby has grown during their stay at the NICU
Premature babies often have longer stays in hospitals and need highly specialized equipment for their complex medical needs. Overnight sleep rooms allow parents to be close to their children while they are being treated. The close proximity also provides parents a chance to learn from the care team how to continue the special care their children will need when they go home.
Centers & Programs
The Miller Children's & Women's Access & Transport Center has a specialized care team to safely transport infants, children, young adults and high-risk expectant mothers who need life-saving specialty care. The team provides the same level of care by ground or air transport that a child or mother would receive at Miller Children’s & Women's – 24 hours a day, seven days a week.
Amazing Babies Program was put in place to bridge the gap between NICU discharge and outpatient care for the most critically-ill babies.
The NICU at Miller Children’s & Women's has an Integrated Transitional Care Area for newborns that need the most attention and require extended care. The Integrated Transitional Care Area within the NICU ensures that patients with a severe diagnosis or pending procedures and surgeries receive special attention and care.
Within our NICU’s Small Baby Unit, we have an Extremely Low Birthweight Program dedicated to micro-preemies.
Parents may have questions or concerns about caring for their infant who is experiencing developmental delays or is transitioning out of the NICU. The expert developmental care team starts building a relationship with the family and the patient during their stay in the NICU and may continue through the age of 3. This ongoing care is provided in a warm, friendly environment.
High-Risk Pregnancy Program provides specialized care to women who are experiencing complications during their pregnancies.
The goal of our Neonatal Continued Care Program is to help your family make a seamless transition. This will be your medical home, specially designed to support recent NICU graduates.
Palliative Care focuses on ensuring the best possible quality of life for patients with a chronic or serious illness. This program addresses the patient’s need for comfort.
During pregnancy, a baby meets growth and development milestones each week. When a baby is born prematurely, they are more likely to experience health problems because they did not spend a full 40 weeks in the womb. Since the baby had less time in the womb, they may have some medical conditions that need to be taken care of in a NICU environment.
Your Care Team
It takes a team of specialty doctors to ensure that a baby’s special needs are met. NICU babies are primarily seen by a neonatologist, but other specialists are often brought over to consult on the baby for their pediatric expertise in specific areas. Neonatologists are pediatric doctors who specialize in the medical care of newborn infants, especially critically ill or premature newborn infants.
Neonatologists









Other Team Members
The NICU at Miller Children’s & Women's is comprised of a multi-disciplinary care team to help meet the needs of premature babies that all receive special training to handle neonates and their families.
Chaplain: A pastor who is available for families to provide them with spiritual assistance.
Interpreter: Language interpreters are available 24/7 at no cost to patients and families. Services include in-person, video and over-the-phone medical interpreters.
Lactation Consultant: A board-certified nurse who has advanced training in breastfeeding management.
Neonatal Case Manager: A registered nurse (RN) who helps with discharge planning and orders home supplies and equipment as needed.
Neonatal Clinical Coordinator: A registered nurse (RN) who is responsible for the NICU’s function for a specific shift. The neonatal clinical coordinator is always available to parents for any questions or concerns.
Neonatal Clinical Nurse Specialist: A specialized registered nurse (RN) who provides clinical consultation, education and assists in coordinating the multi-disciplinary team to help patients and their families.
Neonatal Clinical Social Worker: A professional who provides counseling services to families and assists with emotional, psychological and social support as needed.
Neonatal Hospitalist: A board-certified pediatrician dedicated to the care of newborn infants in the delivery room, Mother/Baby Unit and NICU.
Neonatal Fellow: A pediatrician who is further advancing into the neonatal medicine specialty. This doctor will spend three years in the NICU.
Neonatal Nurse: A registered nurse (RN) who is trained in the care of premature and critically ill babies.
Neonatal Nurse Manager: A registered nurse who has moved into an administrative role, responsible for the overall management and function of the NICU and its staff. The nurse manager is always available to parents for any questions or concerns.
Neonatal Nutritionist: A registered dietitian (RD) with training and experience in planning nutrition for premature and critically ill babies. They ensure that the baby receives adequate calories, protein and essential nutrients to grow.
Neonatal Occupational and Physical Therapists: A professional who specializes in infant development and special feeding problems. They work with families to promote the maximum development needed for their baby’s growth.
Neonatal Pharmacist: A pharmacist checks all medication orders, make recommendations on new drugs, monitor levels and lab work.
Neonatal Respiratory Therapist: A respiratory therapist (RT) who is specialized in infant’s breathing needs, maintains the ventilators, oxygen and gives breathing treatments.
Neonatal Secretary: The smiling ladies at the front desk who will greet, help and answer phone calls.
Neonatologist: A pediatrician with specialized training in the care of premature and critically ill newborns.
Perinatologist: A physician that works with the patient's OB/GYN when complications develop and can provide care for both mom and baby.
Psychologist: A trained psychologist who works with families to deal with the stressors of the NICU environment.
Resident Physicians: A physician who has completed a general internship and is specializing in pediatrics.
Palliative Care Representative: A professional who provides a holistic approach to an infant’s care, providing an extra layer of physical, social and spiritual support. These professionals will help to assure the best quality of life possible for babies and their families.