Joseph Watson was born four weeks early. Unlike many babies born prematurely, Joseph didn’t have to spend time in the neonatal intensive care unit. However, after being home for about two months, his mom Michelle, began to hear wheezing in his chest.
She took him to the doctor and Joseph was given a clean bill of health. But her mother’s intuition told her differently. She found herself at the pediatrician’s office multiple days in a row as she continued to advocate for Joseph.
After a series of tests, Joseph was diagnosed with asthma. By the time he was 2-years-old, Joseph was taking albuterol, which works by relaxing and opening air passages to the lungs to make breathing easier, as well as oral corticosteroids that reduce inflammation and swelling in the airways.
It was at this time that her pediatrician recommended she take Joseph to a pediatric pulmonologist. Many children with asthma can’t get the expert health care they need just by seeing their pediatrician. Asthma requires long-term care and monitoring by physicians who are specifically trained.
Michelle was referred to pediatric pulmonologist Dr. Cyrus Shahriary at the Children’s Pulmonary Institute at MemorialCare Miller Children’s & Women’s Hospital Long Beach.
“The first thing they did was give Joseph an allergy test, and that’s when they told us that Joseph was allergic to almost every common allergen, in addition to his asthma,” says Michelle.
Allergens are substances that cause an allergic reaction. Joseph’s allergy test revealed he was allergic to grass, dust, mold, animals and more. Allergies can commonly trigger asthma, and for cases like Joseph’s, make asthma more severe and difficult to treat.
Because of the complexity of his diseases, Joseph is seen at the Severe Asthma Clinic, which is part of the Children’s Pulmonary Institute. This clinic provides comprehensive, multi-disciplinary care to children struggling with severe asthma. Miller Children’s & Women’s is only one of two hospitals in the state to have this unique program. In one visit at the Severe Asthma Clinic, Joseph is able to see Dr. Shahriary, his pediatric allergist/immunologist Dr. Vincent Devlin, and a team of other medical professionals.
“We categorize a child’s asthma as severe based on their lung function, their symptoms and frequency of symptoms, the need for rescue medication and the level of impairment from everyday activities,” says Dr. Devlin. “For Joseph, the typical treatment plan was not enough to keep his asthma in control. Our collaborative approach and ability to offer him specialized medications has been key to improving his lung function.”
In addition to his standard asthma medications, Joseph was prescribed two biologic medications called XOLAIR® and NUCALA. Biologics target a specific antibody, molecule, or cell involved in asthma.
XOLAIR works by blocking the antibody or substance called Immunoglobulin E (IgE) in the blood. Too much IgE can trigger inflammation of the airways, which can lead to an asthma attack. Similarly, NUCALA works by blocking normal white blood cells in the body called eosinophils. When a person has increased level of eosinophils, it can lead to inflammation in the lungs.
Joseph gets these medications regularly by injection at the Infusion Center at Miller Children’s & Women’s.
“Joseph is the type of kid who is calm and sweet,” says Michelle. “He doesn’t always tell me when he’s not feeling well, but I can tell that he is doing so much better,” says Michelle. “He’s had a lot of good days and has been sleeping through the night more often.”
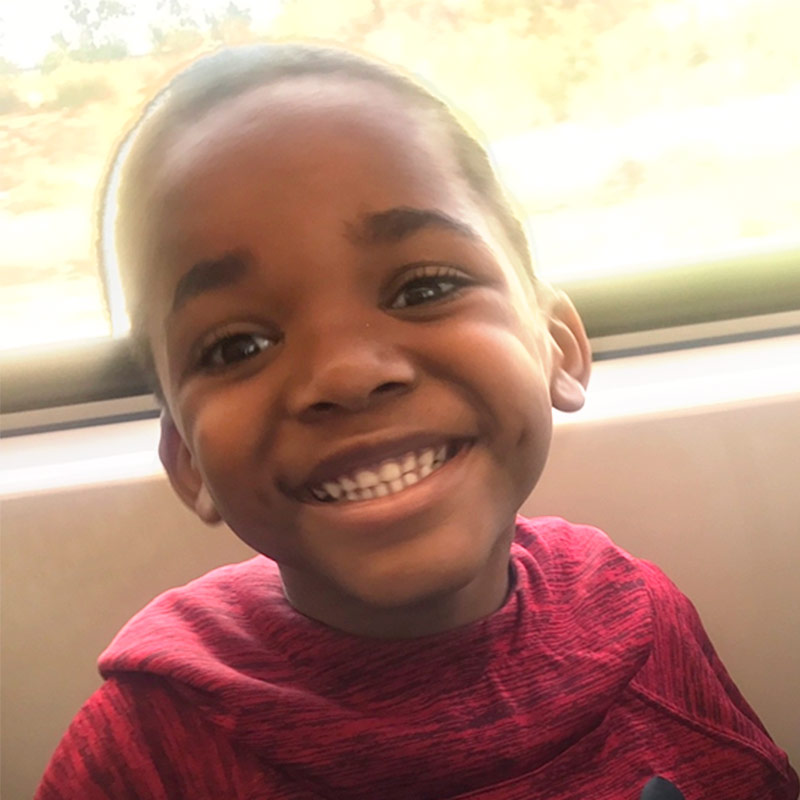
Joseph is now 7-years-old and like many boys his age, he loves gaming, anything to do with technology and building with Legos®. He also puts his lungs to good use with his love of singing.
Joseph’s progress is monitored by the team during his clinic visits. “We use a tool called an asthma control test to help us determine if asthma symptoms are well controlled, and Joseph is now in the ‘well controlled’ range,” says Dr. Devlin.
“At our last visit, Joseph and I were so excited to hear the progress,” says Michelle. “I know there is still room for him to get better, but he has come so far, and I’m grateful for all the support we’ve received.”